HIPAA Certification
Get Free Consultation
Introduction to HIPAA:
The Health Insurance Portability and Accountability Act (HIPAA) is a foundational data privacy law that governs the protection of patient health information. Enacted in 1996, HIPAA aims to safeguard sensitive medical records from unauthorized access and misuse. It ensures that healthcare data is only disclosed with patient consent or under strict regulatory guidelines. For healthcare providers, insurance companies, and business associates, HIPAA compliance is essential to maintain trust, legal integrity, and data security.
HIPAA Certification:
Although HIPAA itself does not issue certifications for compliance, organizations may pursue HIPAA certification through trusted third-party bodies. These entities assess whether an organization’s practices align with HIPAA standards and issue certification to confirm compliance. In many cases, companies also implement frameworks like ISO 27001 Certification alongside HIPAA to strengthen their information security management systems. Together, these certifications provide strong validation that the organization has implemented the necessary safeguards and policies to protect PHI (Protected Health Information).
While HIPAA compliance is mandatory for covered entities (such as healthcare providers, health plans, and healthcare clearinghouses) and their business associates (third-party service providers who handle PHI), not all organizations are required to pursue formal HIPAA certification. However, for organizations that work in the healthcare industry or deal with PHI, achieving certification can provide a competitive edge, minimize risks, and demonstrate a commitment to data security and patient privacy.
How to Get HIPAA Certification:
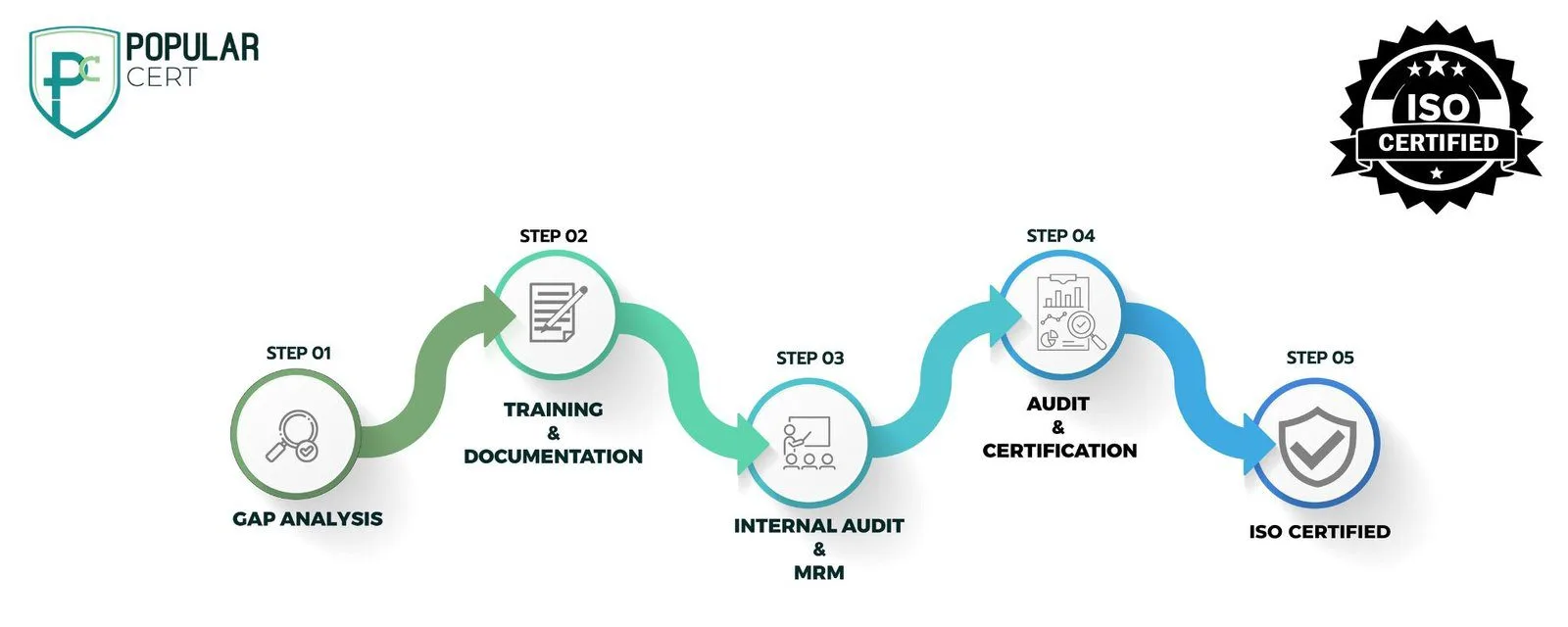
Process of HIPAA Certification
Self-Assessment
One of the first step should be doing a comprehensive self-assessment of the present privacy and security measures at your organization. This includes inquiring about the policy, training of employees, storage of data, and access control in order to identify non-compliance with HIPAA.
Gap Analysis
When the self-assessment has been accomplished, a gap analysis is made to determine the areas in the organization that do not fully comply with HIPAA's regulations. This analysis will serve as a basis for alteration of policies, procedures, and security methods.
Policy and Procedure Updates
According to the conclusions drawn after analyzing the gap, the company revises its internal policies and procedures. Through reworking data security protocols, introducing new privacy safeguards, and ensuring that both the Privacy and Security Rules are adhered to, the organization manages to accomplish that purpose.
Employee Training
Employees must be trained on HIPAA’s regulations, their responsibilities in protecting patient data, and how to handle PHI securely. Training should be conducted regularly to keep employees informed of updates or changes in laws and company policies.
Third-Party Audit and Certification
After implementing changes, a third-party auditor assesses the organization’s compliance with HIPAA standards. If successful, the organization is awarded HIPAA certification, confirming it meets the necessary privacy and security requirements for handling PHI.
Key components of HIPAA
- Privacy Rule: The Privacy Rule is a standard security measure that universally protects health data commencing with its encryption and continuing up to the transfer of information within the healthcare system. Here patients have access to their health information and have the right to control the disclosure of this information.
- Security Rule: This rule is aimed to administer, protect, and maintain the electronic health information by different means of administrative, physical, and technical actions. It specifically tells the company where to encrypt, control access, and do regular checking to guarantee the safety of ePHI (electronic protected health information).
- Breach Notification Rule: The Breach Notification Rule facilitates the protocols to be followed by the entities in case of a data breach that includes PHI. It requires them to notify the patients affected and the Department of Health and Human Services (HHS) if the breach is of over 500 people.
- Enforcement Rule: The Enforcement Rule is a set of provisions that allow for criminal or civil penalties to be applied to those who violate HIPAA regulations. The possible consequences can vary depending on the nature and purpose of the violation.
- Omnibus Rule: This regulation aims to enhance the HIPAA privacy and security protections through amendments arising from the Health Information Technology for Economic and Clinical Health (HITECH) Act. It (the Omnibus Rule) as well broadens the HIPAA scope of business associates and subcontractors.
Types Of Certification
- ISO Certification
- ISO 9001 Certification
- ISO 14001 Certification
- ISO 45001 Certification
- ISO 22000 Certification
- ISO 27001 Certification
- ISO 17025 Certification
- ISO 13485 Certification
- ISO 20000-1 Certification
- ISO 22301 Certification
- ISO 50001 Certification
- ISO 37001 Certification
- IATF 16949 Certification
- ISO 29001 Certification
- ISO 31000 Certification
- ISO 20121 Certification
- ISO 10002 Certification
- ISO 41001 Certification
- CE Mark Certification
- Halal Certification
- BIFMA Certification
- RoHS Certification
- HACCP Certification
- GMP Certification
- Organic Certification
- AS9100 Certification
- TL 9000 certification
- SA 8000 certification
- SoC Certification
- GDPR Certification
- HIPAA certification
Get Free Consultation
Our Clients


















HIPAA Internal Audit Checklist
Benefits of HIPAA Certification
- Enhanced Trust and Credibility: Certification demonstrates a commitment to patient privacy and data security, building trust with clients, partners, and stakeholders.
- Regulatory Compliance: Organizations mitigate the risk of legal penalties and fines by ensuring adherence to HIPAA regulations.
- Data Security and Risk Reduction: Implementing HIPAA safeguards minimizes vulnerabilities, reducing the risk of data breaches and cyber threats.
- Competitive Advantage: Certified organizations gain a competitive edge in the healthcare industry by demonstrating compliance, making them more attractive to potential clients and business partners.
- Improved Operational Efficiency: Implementing HIPAA-compliant policies enhances internal processes, ensuring secure and streamlined data management.
- Business Growth Opportunities: Many healthcare providers and insurers prefer working with HIPAA-compliant organizations, leading to increased business opportunities.
Cost of HIPAA Certification
Cost of HIPAA compliance depends on the size and complexity of the entity and the third-party service provider chosen for the review. Small companies may have less costly audits, whereas big ones with multiplex operations and high data security needs will have cost problems. Costs fall within a range of dealing with third-party audits, consulting with lawyers, training of staff, and the implementation of security measures needed.
Why choose PopularCert for HIPAA Certification
PopularCert should be the top choice for HIPAA certification as it promises a concise process handled by professionals. ISO certification is our core specialization that our team uses to help you deal with HIPAA requirements effectively. We conduct comprehensive evaluations, update policies, train employees and have third-party audits to ensure full compliance. The focus of PopularCert on security and privacy guarantees that your company gets the needed certification, decreased risks, and strict data protection. Our customer-oriented strategy ensures you own customized solutions that satisfy your specific needs as well as comply with all the rules in the long run.
Compliance-Driven for B2B Audience
Stay Compliant. Build Trust. Avoid Penalties.
Get HIPAA certified with Popularcert and safeguard your healthcare operations with confidence.
GET A FREE CONSULTATION NOW
FAQ
What is the use of HIPAA certification?
A company that is HIPAA certified proves that privacy and security standards are being adhered to for (PHI), as well as data protection as well as a reduction in legal risks, which then will result in the trust with the patients and partners.
What is the validity for HIPAA certification?
HIPAA certification does not have an official expiration date. On the other hand, organizations must evaluate and replenish their compliance regularly to keep up with HIPAA’s changing standards and thus protect the patients in the best way possible.
Which organizations must implement HIPAA certification?
If your organization processes the Sensitive Personal Data (SPD), for instance, healthcare sector, health plans, healthcare centers, and associated business partners, you must carry out HIPAA certification to achieve the privacy and security rules.
What happens if an organization does not comply with HIPAA?
HIPAA non-compliance may lead to fines, penalties, and the reputation of the medical provider being undermined. In more serious accusations, you may have to face either civil or criminal penalties for the nature of your violation.
How often should HIPAA compliance be reviewed?
To guarantee the observance of the latest standards and reduce possible vulnerabilities, organizations should periodically check their HIPAA compliance with the help of audits, risk assessments and staff training—that is, at a minimum frequency of once a year.
